What is Gastric Sleeve Surgery
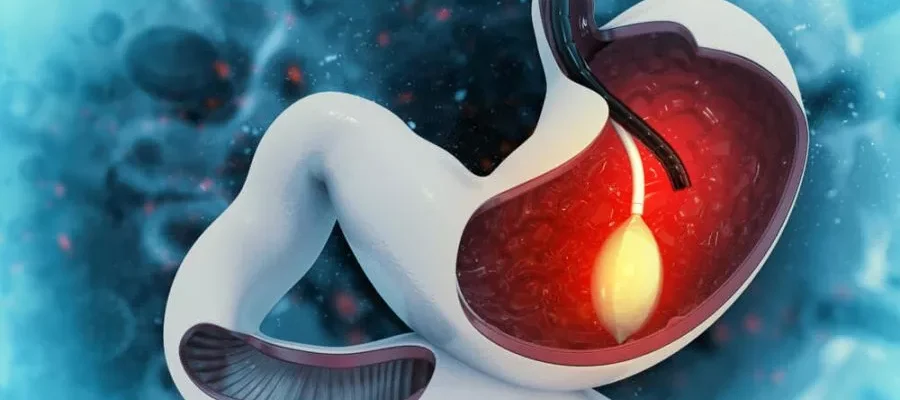
The term “sleeve gastrectomy,” often known as the “gastric sleeve procedure,” may be what you’re looking for. The stomach is surgically divided into a smaller “sleeve” and a larger “tubular” section in order to facilitate weight reduction. The operation permanently lowers stomach size, which often leads to substantial weight loss and the improvement or resolution of health problems associated with obesity.
The quantity of food a person can eat is restricted since the stomach size has been decreased. This causes the individual to feel full on a very modest quantity of food.
The hormones in the digestive tract that regulate appetite, fullness, and blood sugar levels are all affected by the operation. Hormonal shifts may make people feel full sooner after eating less food.
To reiterate, the patient’s dedication to a new lifestyle is crucial to the success of this procedure. Maximizing weight reduction and keeping it off after surgery requires a commitment to a tight diet and frequent physical exercise.
Why would you need a tube in your stomach?
Several medical conditions need the insertion of a tube into the stomach. People who are unable to take in enough food or liquid via their mouths may be given nourishment, fluids, and medicines through these tubes, also known as feeding tubes or gastrostomy tubes (G-tubes). Some examples of situations in which a stomach tube might be necessary are as follows:
Stroke, certain neurological illnesses (such as Parkinson’s disease, multiple sclerosis), or malignancies of the head and neck may all impede a person’s ability to swallow, a condition known medically as dysphgia.
Cancer, AIDS, and other chronic diseases may induce malnutrition because the body may need more nutrients than the individual is getting, or because the person is eating less as a result of the illness or its treatment.
Esophageal Conditions: Esophageal strictures or atresia are two examples of problems that might need a G-tube to facilitate nutrition.
Feeding tubes are often used to treat gastrointestinal motility disorders such gastroparesis, in which the stomach does not empty food adequately.
Babies born prematurely or with certain medical issues may need supplemental feeding until they are able to feed orally.
In the case of oral or facial surgery, the patient may be temporarily unable to consume food or liquids, necessitating the use of supplemental nourishment.
Nutrition and hydration may be administered via a feeding tube to patients in a vegetative condition or with impaired awareness.
Patients who need prolonged mechanical breathing may have a feeding tube inserted to avoid malnutrition and aspiration.
Patients who have a significant risk of aspirating food or liquids into their lungs may benefit from receiving nourishment via a feeding tube.
Because of birth defects known as congenital anomalies, some newborns are born unable to swallow.
Can a stomach tube be removed?
It is possible to remove a PEG tube or other kind of stomach tube. The procedure for removal and subsequent treatment will be tailored to the specifics of each patient, tube type, and length of time in place. For context, consider the following:
Tubes Placed for a Limited Time Period If the tube has only been in place for a short period of time, removing it should be a simple process. Most of the time, you can just take the tube out gently and cover the wound with some clean gauze. In most cases, the stoma, or tiny opening, will seal on its own within a few days.
Stomas that have been left open for a long period may need extra time to heal on their own, or perhaps surgery, to shut. To hasten the closure of the tract, a smaller tube or a specific dressing may be substituted for the larger one.
The actual procedure of removal is often short and painless. After the region surrounding the tube has been cleansed, the tube itself is gently withdrawn after the balloon has deflated. After that, a clean bandage is placed over the area.
Aftercare is keeping the affected region clean and looking out for symptoms of infection including redness, swelling, pus, or a high temperature. A few days to a few weeks of close observation may be required to make sure the spot heals correctly once the tube has been removed.
Professional Medical Advice: Have a doctor do or oversee any removal procedures. When and how the tube should be withdrawn, as well as any aftercare instructions, should be discussed with a medical professional.
How long does a gastric tube last?
The longevity of a gastric tube, also known as a gastrostomy tube or G-tube, is contingent on the tube’s design and construction, although it is intended for long-term usage. For context, consider the following:
Common G-tube materials include silicone and polyurethane. They have an average lifespan of 3 months to 6 months. The G-tube’s anchoring balloon (if present) might degenerate with time and eventually need to be replaced. Both the valve mechanism and the tube itself might eventually wear out and need replacing
Buttons, or low-profile G-tubes, are similar to regular catheters except that they sit flush with the skin. Depending on the model and the manufacturer’s recommendations, their lifespan may be anywhere from three months to a whole year.
Some tubes, known as JE-tubes, go from the stomach all the way to the jejunum, the first segment of the small intestine. Due to their greater length and increased likelihood of wear and tear, jejunostomy tubes (JE-tubes) may not survive as long as conventional G-tubes. They may live for a few weeks or a few months at the most.
The usefulness of a G-tube may be affected by many variables:
Tube longevity may be increased with regular cleaning and maintenance.
More wear and tear on the tube may occur in physically active people.
Silicone tubes are more pleasant for some patients because they are more flexible, but they may wear out more quickly than polyurethane tubes.
How long can a feeding tube stay in?
The kind of feeding tube used and the patient’s particular requirements will determine how long the tube may remain in place. The following is a broad outline:
These tubes, known as nasogastric (NG) tubes, are placed in the nose and go down the esophagus into the stomach. They are intended for brief periods of time, anything from a few days to a few weeks. Nasal or esophageal irritation, ulceration, or sinusitis have been linked to long-term usage.
NJ tubes are similar to NG tubes, except they continue into the stomach and into the small intestine. They are intended for temporary usage, similar to NG tubes, and should be removed after a few weeks at the most.
Long-term stomach tubes called gastrostomy tubes (G-tubes) are placed via surgical incision in the abdominal wall into the stomach. If taken care of, they have a long lifespan (months to years). The precise duration is determined by the tube’s material, the manufacturer’s specifications, and the care given to the tube. Due to normal wear and tear, G-tubes may need to be replaced at regular intervals.
J-tubes, or jejunostomy tubes, are surgically implanted through the abdominal wall into the jejunum of the small intestine. They are designed for prolonged usage, like G-tubes, but owing to their location and the nature of delivering feedings straight into the small intestine, they may need replacement more regularly.
G-tubes of the PEG (Percutaneous Endoscopic Gastrostomy) kind are inserted endoscopically. They can be left in place for a while (months to years), but they may eventually need to be replaced or tweaked.
Are gastric tubes permanent?
Despite their name, gastric tubes (also known as gastrostomy tubes or G-tubes) are not permanent and may be removed at any time. When they are no longer required or if issues emerge, they may be eliminated. A summary is as follows:
G-tubes, depending on the patient’s condition and the kind of tube used, may be left in place for anything from a few months to a few years. The tube may eventually wear out or become damaged beyond repair. However, the tube may be withdrawn if the underlying cause for its installation goes away or if another technique of feeding proves to be more suitable.
In most cases, a G-tube may be removed with little effort. If a balloon is keeping the tube in place, deflating it will allow you to carefully remove the tube. The resultant skin opening (called a stoma) often heals on its own after some time, however some patients, particularly those who have had their tube in for an extended period of time, may need modest surgical intervention to assure full closure.
Some individuals may need tube feedings permanently because their illnesses prevent them from swallowing or ingesting enough food orally. In certain circumstances, a G-tube or other feeding tube may be required for the rest of the patient’s life. However, even in these cases, the tube device itself will eventually need to be replaced owing to normal wear and tear.
Why do doctors put feeding tube in stomach?
When a patient is unable to take in enough food or liquids via their mouth, doctors will insert feeding tubes into their stomach or intestines to provide the necessary nutrients, fluids, and medicines. Some typical indications for inserting a feeding tube include:
Conditions such as strokes, certain neurological illnesses (such as Parkinson’s disease, multiple sclerosis, or amyotrophic lateral sclerosis), or malignancies of the head and neck might compromise a person’s ability to properly swallow.
Coma Decreased Consciousness: A feeding tube may be necessary to provide enough nourishment and hydration for patients in these states.
Oral nutrition may need to be adjusted momentarily after trauma or surgery to the face, jaw, or mouth.
For patients with gastrointestinal conditions including gastroparesis (slow stomach emptying) or severe esophageal reflux, an alternative feeding route may be necessary.
Chronic malnutrition occurs when a person does not get enough of the nutrients they need because they are either unable to eat enough or their appetite decreases as a result of their disease or its treatment.
Babies who are born prematurely or who have specific congenital disorders may need feeding tubes to get nutrients until they are able to feed themselves orally.
Patients who are at danger of aspirating (inhaling food or fluids into the lungs) may benefit from receiving nourishment via a feeding tube.
Patients who need to rely on mechanical ventilator for an extended period of time may need a feeding tube to avoid malnutrition and prevent aspiration.
Some people, particularly children with severe developmental or behavioral issues, may have a complete inability to eat via their mouths or a complete refusal to do so.
What are the side effects of tube feeding?
Nutrition is delivered to the stomach or small intestine through a tube in tube feeding, sometimes called enteral nutrition. It’s meant for those who, for different reasons, can’t eat normally. Tube feeding, like any other medical procedure, may have unwanted consequences in certain patients. Among the potential negative outcomes are:
When food goes into the lungs instead of the stomach, this is called aspiration. Pneumonia and other respiratory problems are possible outcomes.
Nausea, vomiting, diarrhea, constipation, bloating, and cramps are all symptoms of problems in the digestive tract.
Electrolyte imbalances, including low phosphorus, potassium, and magnesium levels, characterize refeeding syndrome, a potentially fatal illness that may arise when feeding is started in a malnourished individual.
Dehydration and electrolyte imbalances are two examples of metabolic disorders.
Problems caused by the tube:
The tube becomes dislodged or moves.
The tube has become clogged or blocked.
Infection at the place where the tube was inserted.
Red, rough granulation tissue (from where the tube was removed) surrounds the area.
If the tube is inserted via the nose, it may cause erosion or pain.
Erosion or ulceration of the stomach or duodenum.
There is a chance of either overfeeding or underfeeding, both of which might cause metabolic problems or nutritional deficiencies.
There is a possibility that tube-fed drugs are not absorbed as well as orally administered ones.
Some patients may feel embarrassed by the tube, which may cause them to withdraw socially or have other negative psychological effects.
Tube feeding formula intolerance may occur if a patient is allergic to or sensitive to one of the ingredients in the formula.
Formula may remain in the stomach for longer than necessary if gastric emptying is delayed.
